
- Posted: February 22, 2021
- |
- TheraNest Team
What is the 8 Minute Rule for therapy billing? A large portion of mental health organizations submit claims to Medicare on a regular basis. This means that they should be familiar with the 8-minute rule for billing. While many providers are familiar with this, they have yet to perfect the process. In fact, many providers are flustered by its boundaries and battle with adhering to the rule. Understanding how this rule works and how to perfect its process will only help therapists improve their bottom line.
What is the 8 Minute Rule for Therapy Billing?
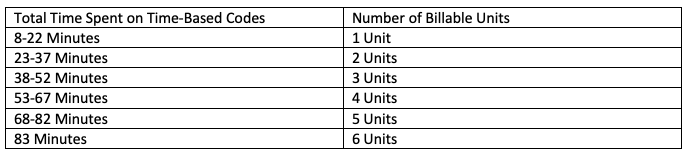
Billing units can be split into two categories: Service-Based CPT (Common Procedural Technology) codes and Time-Based CPT codes. The 8-minute rule for therapy is a time-coded stipulation that allows providers to bill Medicare insurance payers for one billing unit of service. Time-based codes are determined by the amount of time a provider spends with a client in which they are delivering services that are tied to that code. Calculating these types of billing units can be frustrating, especially when time spent with a patient does not break down into perfect increments. CPT guidelines state that time-codes should be broken down into 15-minute increments. When the time does not divide evenly into 15-minute segments, the 8-Minute Rule for therapy billing applies. It is what payers use to determine the number of units a provider should bill for.
While this rule originated under Medicare, many private payers use it to measure billing units to this day. It has become the standard to time-coded billing units. One of the most confusing aspects of this type of code is when it applies versus when it does not.
Breaking Down Treatments into Units:
Short Treatments:
When a treatment lasts shorter than 8 minutes, the 8-minute rule does not apply. When this happens, providers have to bill a little differently. They should add up the total time spent on all short treatments. For example, if the treatments each add up to 5, 6, and 7 Minutes, one unit may be billed for the service that was 7 minutes long. Although the total number of minutes adds up to 18, they still only get to bill for one unit. In order to bill for more units, the provider needs to spend at least 8 minutes of time on each service, following the 8-minute Rule for therapy billing.
Multiple treatments Lasting Longer Than 8 Minutes:
Now, if a provider offers multiple treatments that are at least 8 minutes, the 15-minute threshold needs to be considered. They need to add up the total number of minutes spent on services and divide that by 15. For example, if a provider offers services lasting 9, 10, 11 minutes, they need to add up all of the minutes and divide by 15. 30 minutes divided by 15 equals 2 billable units.
Billing for the 8 Minute Rule:
Example of when the 8 Minute Rule Applies:
In this example, a provider spends a total of 74 Minutes with the patient doing a number of different evaluations and exercises. The provider needs to break down the number of minutes spent on each exercise to determine how many units they can bill for. In this scenario, the session can be broken down into 30 minutes, 30 minutes, 9 minutes, and 5 minutes. Each increment spent on a different exercise. How many units can the provider bill for this one-hour session?
The answer is 5 billable units. This is because the first two services add up to 60 minutes and can be broken down into 4 perfect 15-minute increments, allowing them to bill for four units. The remaining 14 minutes of services have to be applied to the 8-minute rule for therapy billing. One of the services was at least 8 minutes, allowing them to bill for another unit. The last service, however, only lasted 5 minutes, making it not billable under the 8-minute rule for therapy billing. This means that the provider could bill for 5 total units.
While the 8-minute rule for therapy billing can be complicated, understanding it can help a provider greatly improve their bottom line.
With a dedicated billing specialist at your side, your practice can perfect its behavioral health insurance billing.

